Practice Essentials
Atherosclerotic risk factors have been evaluated in multiple longitudinal epidemiologic studies, such as the Framingham Heart Study. These studies have defined advancing age, male sex (or better stated, the absence of protective female hormones), hypertension, dyslipidemias, diabetes, cigarette smoking, and family history as predictors of subsequent cardiac events and angiographically demonstrated coronary artery disease. [1, 2, 3]
When x-rays were discovered, calcium was again recognized as a disease marker. In fact, for most of the 20th century, calcium, because of its density, was the only feature that stood out on radiographs of the heart. In the 1950s, heart disease became more recognized as a significant cause of mortality in the United States. Along with this recognition came numerous publications about the ability to detect calcifications in the coronary arteries with radiography. In some ways, this period can be thought of as the first age of importance for calcium detection in the heart.
This period came to an end with the widespread acceptance of coronary angiography and other less invasive tests, such as stress thallium testing. If an actual stenosis or area of ischemia could be detected, attempts to qualitatively detect calcium with radiography or fluoroscopy seemed primitive. The advent of angioplasty and stent placement in the treatment of arterial stenoses seemed to herald the end of calcium detection.
Tremendous overlap exists, and sensitivities and specificities vary, even when multiple risk factors are applied. Novel risk factors have been proposed in an effort to enhance disease detection, particularly in asymptomatic patients. As a result, clinicians now may measure levels of homocysteine, fibrinogen, lipoprotein subunits (eg, lipoprotein A), C-reactive protein, and other biochemical markers of coronary atherosclerosis and subsequent cardiovascular events.
There are 3 primary reasons why detection of calcification in the coronary arteries is of primary importance. The first and foremost reason is that calcium is a marker for a diseased artery.
The second reason has to do with the revolution in CT scanning. Electron-beam CT (EBCT) was the first technique to provide a real breakthrough in the quantitation of calcium in the coronary arteries. Although this examination is valuable, the cost of the machines limited its use, and, by association, its impact. Some time afterward came helical, or spiral, CT. This technique was further improved with the addition of twin- and even quad-detector arrays. These machines allowed truly fast, completely noninvasive examination of the average person. During this period, the scanners were still not quite sophisticated enough to allow direct visualization of the coronary arteries while filled with contrast material. This continued to focus attention on the capabilities and significance of calcium scoring.
Advances in CT technology continued with the development of 16- and 64-slice scanners. With these scanners, more attention was directed to coronary artery CT angiography, but the use of calcium scoring in preventive cardiology had solidified. Newest scanner have 320 detector rows that allow imaging of a larger area of the body at one time, and the gantry (the doughnut-shaped part) can complete a full rotation in 275 milliseconds. In addition, the newest scanners substantially reduce radiation exposure. [4]
The third reason is mortality from heart disease. Cardiovascular disease is the leading global cause of death, accounting for more than 17.9 million deaths in 2015. That number is expected to increase to close to 24 million by 2030. In the United States, over 366,000 people die each year of coronary artery disease. [1]
(See the CT scan images of coronary artery calcification below.)
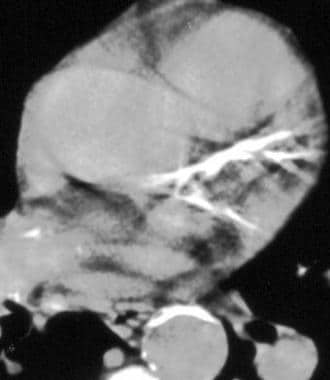
 Coronary artery calcification - CT. Cross-sectional image obtained through the heart at the level of the left anterior descending (LAD) artery. The protocol on the CT machine colors all structures with an attenuation of greater than 130 HU pink. No calcium (pink) is present in the LAD or diagonal branch.
Coronary artery calcification - CT. Cross-sectional image obtained through the heart at the level of the left anterior descending (LAD) artery. The protocol on the CT machine colors all structures with an attenuation of greater than 130 HU pink. No calcium (pink) is present in the LAD or diagonal branch.
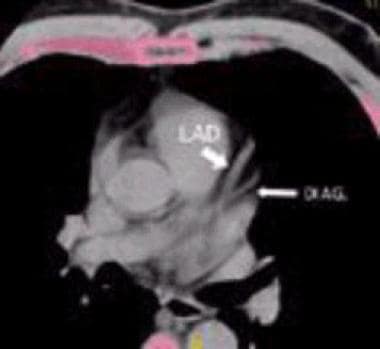
 Coronary artery calcification - CT. Image obtained in a patient with a large amount of calcium in the left anterior descending (LAD) artery. Note that other hyperattenuating structures (eg, bone, calcified lymph nodes) are pink. During the scoring process, the radiologist must circle only those areas that correspond to one of the coronary arteries.
Coronary artery calcification - CT. Image obtained in a patient with a large amount of calcium in the left anterior descending (LAD) artery. Note that other hyperattenuating structures (eg, bone, calcified lymph nodes) are pink. During the scoring process, the radiologist must circle only those areas that correspond to one of the coronary arteries.
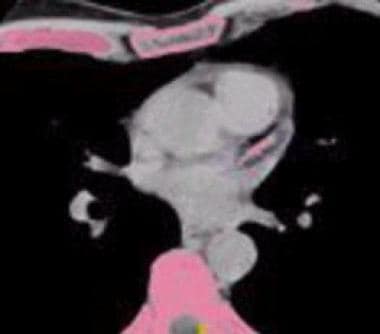
 Coronary artery calcification - CT. Image obtained without the threshold set to color the calcium pink. Note the large amount of calcium in the left anterior descending (LAD) and left circumflex arteries.
Coronary artery calcification - CT. Image obtained without the threshold set to color the calcium pink. Note the large amount of calcium in the left anterior descending (LAD) and left circumflex arteries.
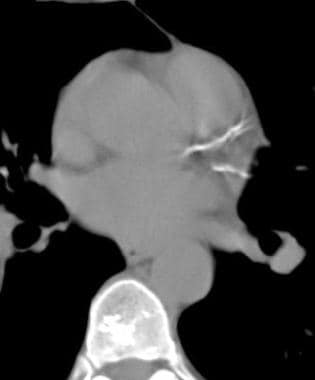
 Coronary artery calcification - CT. Section caudal to that in the previous image shows calcium in the left anterior descending (LAD) artery as it courses down the front of the heart. The vessel is now depicted in cross section.
Coronary artery calcification - CT. Section caudal to that in the previous image shows calcium in the left anterior descending (LAD) artery as it courses down the front of the heart. The vessel is now depicted in cross section.
Conventional CT demonstrates calcification in 50% more vessels than fluoroscopy does in patients with angiographically proven stenosis. However, conventional CT has a slow scan time and is prone to artifacts from cardiac and respiratory motion and volume averaging.
Electron-beam CT (EBCT) minimizes motion artifacts, because cardiac-gated imaging can be triggered by the R wave of the cardiac cycle. Imaging can be performed in diastole, minimizing cardiac motion. Typically, 20 contiguous, 100-millisecond, 3-mm thick sections are obtained during 1 or 2 breath-holds, and coronary artery calcification is observed as a bright white area along the course of coronary vessels. [5]
Helical scans are performed with acquisition times approaching 0.5 second to 250 milliseconds. Calcific deposits are identified as bright white areas along the course of coronary arteries (see the image above). [4]
Pathophysiology of calcium in coronary arteries
Coronary artery calcification is a recognized marker for atherosclerotic coronary artery disease (CAD) and can begin in patients as young as 10-20 years. The calcification itself is calcium phosphate (hydroxyapatite), which is similar to that in bone. [6]
In an early study of autopsy findings in 2,500 patients, calcium in the coronary arteries and the total plaque burden were shown to be correlated. Patients who died of coronary artery disease were found to have 2-5 times as much calcium as those who died of other causes.
The American College of Cardiology (ACC) and American Heart Association (AHA) Consensus Panel have noted that coronary calcium is part of the development of atherosclerosis and occurs exclusively in atherosclerotic arteries and is absent in the normal vessel wall.
Atherosclerotic risk factors have been evaluated in multiple longitudinal epidemiologic studies, such as the Framingham Heart Study. These studies have defined advancing age, male sex (or better stated, the absence of protective female hormones), hypertension, dyslipidemias, diabetes, cigarette smoking, and family history as predictors of subsequent cardiac events and angiographically demonstrated coronary artery disease.
Multiple angiographic and epidemiologic studies have shown that the mechanism of myocardial infarction and/or sudden cardiac death in asymptomatic patients is plaque rupture with superimposed thrombosis. In most cases, the plaque burden is not flow limiting; therefore, the patient does not have a positive stress-test result or even a significantly abnormal coronary angiogram.
Coronary Artery Calcium Scoring
Coronary artery calcium scoring (CACS) is a measure of coronary artery calcification detected on EBCT or helical CT. It is a marker of the atherosclerotic plaque burden and is an independent predictor of future myocardial infarction and mortality. CACS provides incremental risk information beyond traditional risk calculators. [5, 7, 2]
To calculate a CAC score, the original Agatston method involved defining a calcified lesion as a density ≥130 Hounsfield units and an area ≥3 pixels. A score was assigned to each lesion (the product of density and area), and the total score was reached by adding up each of the calcified lesion scores. A semiautomated method is now commonly utilized, following the same principles. [5]
Cardiovascular risk stratification using calcium scoring has been widely studied, and standard categories according to cardiovascular prognosis and total mortality are as follows [8] :
CAC=0: very low risk of death (< 1% at 10 years)
CAC=1-100: low risk of death (< 10% at 10 years)
CAC=101-400: intermediate risk of death (10-20% at 10 years)
CAC=101-400 and >75th percentile for age, sex, and ethnicity: moderately high risk of death (15-20% at 10 years)
CAC >400: high risk of death (>20% at 10 years
In a large study of asymptomatic patients who underwent a coronary artery calcium (CAC) CT scan, a high CAC score predicted a higher risk of death during a mean follow-up of 12 years. Compared with individuals with a CAC of 0, those with a CAC >400 had a 1.8-fold to 3.2-fold increased risk of all-cause death and a 3.1 to 5.1-fold increased risk of CVD death. [9]
Electron-Beam and Helical CT Scanners
The initial investigation of coronary artery calcification with CT was made possible with the development of the electron-beam CT (EBCT) scanner in the late 1980s. The speed of this machine was vastly superior to that of existing CT scanners. With this speed, it had the ability to "stop" heart motion enough to allow measurement of the amount of calcium in a coronary artery. Another revolution in CT has was the development of ultrafast spiral CT. [10, 11]
Principles of EBCT
One of the factors that limit the speed of a conventional CT scanner is necessary rotation of the tube around the patient. EBCT completely avoids this problem because the machine does not have any moving parts. A beam of electrons is generated and then focused with a series of electromagnets. The beam is directed onto 1 of 4 tungsten targets under the patient. The resultant fan-shaped x-ray beam passes through the patient and is collected by a 210° arc of detectors above the patient. More than 3,000 detectors are used in this process.
EBCT allows the acquisition of 1.5- to 3-mm sections, with an exposure time of 100 milliseconds. The images are gated to the end of diastole, and the entire examination is performed during 1 breath-hold by the patient. Usually, 40-60 sections are obtained with this method.
Principles of multisection helical CT
Helical, or spiral, CT has renewed interest in many applications for CT. The major advantage of this technique is that it is faster than conventional CT. In addition, CT manufacturers have been able to put as many as 320 sets of detectors into the conventional donut configuration.
During a single-section spiral CT examination, the patient moves at a rate of about 5 mm/s while the tube rotates at a rate of up to 3 revolutions per second. Typically, a scanning length of 8-11 cm is used. Most existing spiral scanners are capable of a sub 100-ms acquisition time. Although this still hasn't equaled the original temporal resolution of EBCT, the other aspects of the multislice scanners make them overwhelmingly better. All major CT manufacturers now have 128-slice or greater machines available, with the latest being 320-slice.
Technique
Although each manufacturer has different protocols, the basic techniques are similar. No patient preparation is required. Blood samples do not have to be obtained, and no contrast material is used. Some manufacturers recommend the removal of any metal object that may be near the chest region. Examples include metal buttons, bras with underwires, and necklaces. Metal objects are removed because they cause non-linear x-ray scatter that can produce artifacts in the images.
Asking patients to practice holding their breath may be helpful, not because a long breath hold is needed (usual duration, 15-30 s), but because reproducibility of their breath-holding is enhanced. Many centers ask the patient to complete a risk-assessment questionnaire to aid in the overall interpretation of the study. The patient lies supine on the scanner gantry with the arms over the head. If the patient cannot raise the arms, an acceptable scan can be obtained with the patient's arms at his or her sides.
Settings for the scanner depend on the manufacturer's recommendations. A typical protocol for a quad-slice multidetector CT would be 165 ma, 120 kVp, 0.5 pitch, and quad X 2.5 mm.
The use of cardiac gating is an area of current disagreement. Some manufacturers do not use it at all, while others disagree about whether it should be used prospectively or retrospectively. Although the addition of gating is not difficult, it requires more patient preparation than that of the simple CT scanning. Leads must be placed on the patient's chest; at some centers, the patient may need to wear a hospital gown.
Results
Coronary segments with a luminal obstruction of greater than 50% are likely to have some calcification that is detectable with electron-beam CT (EBCT). In one trial, a 0 calcium score had a 100% predictive value in the exclusion of angiographic evidence of obstructive epicardial coronary lesions. The higher the calcium score, the more likely the presence of angiographic obstructive disease. In another study, [12] a calcium score greater than 371 had a 90% specificity in the detection of a luminal obstruction of greater than 70%. Specificity tends to decrease with advanced patient age, but it increases with the number of calcified vessels as well as the total calcium score. [13]
In a study in which calcium scores and thallium stress test results were compared, almost one half of the patients with scores greater than 400 had a normal thallium stress result. [14] Such testing may not be contradictory in terms of the pathophysiology; thallium detects inducible ischemia, not plaque burden.
Coronary calcification is strongly associated with the prognosis. Indeed, the extent of coronary atherosclerosis (total calcium score) is the most powerful predictor of subsequent or recurrent cardiac events. This was true in the early days when calcium was detected with fluoroscopy and conventional CT.
When EBCT calcium scores became available, the prognostic value of coronary calcification was again affirmed. The higher the calcium score, the worse the prognosis. [15, 16, 17] The degree of coronary calcium was a good predictor of the development of symptomatic cardiovascular disease. In a study by Agatston et al, the mean calcium score for patients with a cardiovascular event was 399, compared with a mean score of 76 in those without such an event. One study suggested that the detection of coronary calcification at EBCT was a better predictor of subsequent events than many traditional risk factors, including those evaluated in the Framingham database. [18]
Cardiac events do occur in patients with low calcium scores, but the incidence is low. Intravascular ultrasonographic studies show that as many as 30% of coronary plaques are devoid of calcium. In an autopsy study, [19] the benefit of combined assessment of coronary artery calcification and risk factors (Framingham Risk Index) in predicting sudden cardiac death was apparent. In the study, 79 consecutive adults with sudden cardiac death were evaluated by using a Framingham Risk Index and histologic findings of coronary calcification. The risk classifications with the 2 techniques agreed in a majority of the patients. Patients with plaque erosion (as opposed to plaque rupture) who were dying of sudden cardiac death had significantly less coronary calcification and lower Framingham Risk Indexes.
Clearly, in establishing the cardiac risk, traditional coronary artery disease risk factors and coronary calcification may be most useful when used in combination. Whether risk stratification is further enhanced with the use of novel risk factors is yet to be determined. [15, 20, 21, 22]
Questions & Answers
Overview
What are atherosclerotic risk factors?
Why is detection of coronary artery calcification important?
What is the role of CT in the detection of coronary artery calcification?
What is coronary artery calcium scoring (CACS)?
What is the role of electron-beam CT (EBCT) in the detection of coronary artery calcification?
What is the role of multisectional helical CT in the detection of coronary artery calcification?
How is electron-beam CT (EBCT) performed in the detection of coronary artery calcification?
Which findings on electron-beam CT (EBCT) are characteristic of coronary artery calcification?
-
Coronary artery calcification - CT. Cross-sectional image obtained through the heart at the level of the left anterior descending (LAD) artery. The protocol on the CT machine colors all structures with an attenuation of greater than 130 HU pink. No calcium (pink) is present in the LAD or diagonal branch.
-
Coronary artery calcification - CT. Image obtained in a patient with a large amount of calcium in the left anterior descending (LAD) artery. Note that other hyperattenuating structures (eg, bone, calcified lymph nodes) are pink. During the scoring process, the radiologist must circle only those areas that correspond to one of the coronary arteries.
-
Coronary artery calcification - CT. Image obtained without the threshold set to color the calcium pink. Note the large amount of calcium in the left anterior descending (LAD) and left circumflex arteries.
-
Coronary artery calcification - CT. Section caudal to that in the previous image shows calcium in the left anterior descending (LAD) artery as it courses down the front of the heart. The vessel is now depicted in cross section.
-
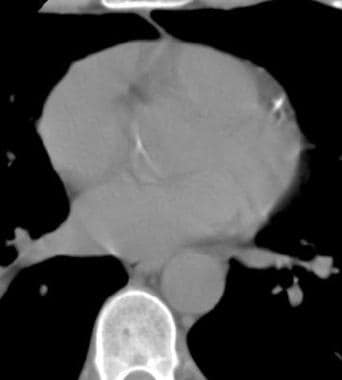
Helical non–contrast-enhanced CT reveals calcification involving the left main coronary artery.